Pikralida and the Nencki Institute of Experimental Biology , Pikralida are working on a breakthrough therapeutic solution preventing the development of epilepsy following brain injury or stroke. The article about this exciting project has been published today at Biotechnologia.pl website.
Authors: Professor Leszek Kaczmarek (Nencki Institute of Experimental Biology of the Polish Academy of Sciences, Warsaw), dr Barbara Pijet-Binkiewicz (Nencki Institute of Experimental Biology of the Polish Academy of Sciences, Warsaw), dr Anna Krause (Pikralida sp. z o.o.), dr Joanna Lipner (Pikralida sp. z o.o.)

Epilepsy is a chronic neurological disease involving recurrent epileptic seizures, which are a manifestation of temporary brain function disorder consisting of excessive and abrupt spontaneous bioelectrical discharges in nerve cells. Currently, approximately 30% of epilepsy cases are incurable, and chronic drug treatment is necessary to relieve the symptoms thereof. The occurrence of epileptic seizures, as well as the continuous medication, means significant limitations in terms of both professional and social life for the patients.
Epilepsy may manifest at any age, although it has its onset usually before the age of 20, while in adults it can develop as a complication following a brain injury or stroke. The first episode usually occurs within the first two years after the incident and affects 5 to 30% of people. The more severe and extensive the injury, the more likely it is that epilepsy will develop. It is estimated that every year in Europe and in the United States there are 2.3 million serious head injuries and 1.9 million strokes, each of which may result in the onset of epileptogenesis ultimately leading to epilepsy.
Epileptogenesis is a continuous and long-term process, during which the normal brain network is functionally altered toward increased susceptibility to epileptic seizures. This process generally increases the risk of spontaneous recurrent epileptic seizures. There are two stages of epileptogenesis. The first is the period before the onset of status epilepticus, and the other involves the development of epilepsy with full-fledged symptoms, namely spontaneous, repetitive seizures. In most cases, epilepsy is caused by factors such as brain injury, including stroke, traumatic brain injury, or status epilepticus (SE). These may be due to structural or metabolic causes. The development of epilepsy over time varies depending on the type of brain injury. The epilepsy develops fastest after SE onset and following stroke.
Together with the Nencki Institute of Experimental Biology, Pikralida is working on a breakthrough therapeutic solution preventing the development of epilepsy following brain injury or stroke. The project is based on the results of long-term studies on the role of the enzyme MMP-9 in the development of epileptogenesis, conducted under the supervision of Professor Leszek Kaczmarek, head of the Laboratory of Neurobiology at the Nencki Institute of Experimental Biology of the Polish Academy of Sciences.
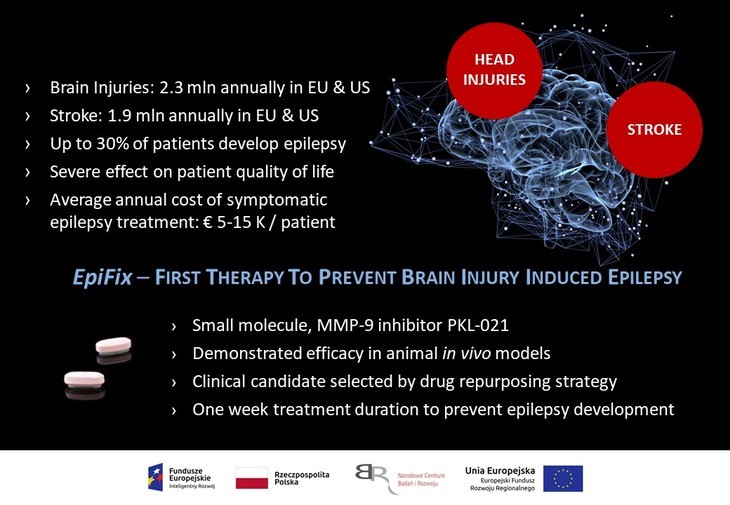
The candidate drug was selected by way of a reposition strategy of a clinical candidate whose development had been discontinued in the past due to lack of efficacy in the originally developed indication. The inhibitor of matrix metalloproteinase 9 (MMP-9) named PKL-021, selected during the screening is a low molecular weight chemical compound having high activity and optimal drug-like properties. The therapeutic potential of the compound has already been confirmed in mouse models of epileptogenesis and will be tested in further in vivo models.
The involvement of MMP-9 in proliferation, maturation, angiogenesis and immune response has been previously demonstrated. MMP-9-induced breakdown and degradation of extracellular matrix proteins is also known for its effect on the prevention and induction of diseases such as cancer, cardiovascular disorders, autoimmunity and neurodegeneration. Research headed by Professor Leszek Kaczmarek also suggested that MMP-9 may play a significant functional role in synaptic plasticity of the brain. Plasticity is behind the changes in the functioning of neuronal networks, allowing them (and thus the brain) to adequately respond to changing environment and, consequently, the appropriate response of the body. Physiologically, synaptic plasticity underlies e.g. learning and memory, whereas under pathological conditions, abnormal plasticity underlies the most serious neuropsychiatric conditions, including autism spectrum disorders, schizophrenia, and epilepsy development. The importance of the involvement of MMP-9 in these conditions has been repeatedly demonstrated by various research groups working on animal models.
MMP-9, or extracellular matrix metalloproteinase, is a zinc-dependent endopeptidase that together with MMP-2 forms the gelatinase family. MMP-9 is expressed e.g. in neurons during cell excitation and makes part of a larger molecular system active at single synapses which regulates their function. Led by Professor Leszek Kaczmarek, head of the Laboratory of Neurobiology at the Nencki Institute of Experimental Biology of the Polish Academy of Sciences, scientists from the Institute are researching the role of MMP-9 in various processes such as epilepsy development.
Studies on the development of epilepsy (epileptogenesis) in animals first showed an increase in MMP-9 activity in this process, and then the effect of MMP-9 on the development of epileptogenesis was clearly demonstrated, using genetically modified mice and rats. Importantly, prolonged epileptic seizures are associated with high serum levels of MMP-9 in humans, so that lowering its levels may result in reducing/blocking subsequent seizures. The therapeutic potential of PKL-021 and the possibility to use it as a treatment preventing the development of post-injury and post-stroke epilepsy may be confirmed by conducting Phase II Proof-of-Concept clinical trials on a patient population. To achieve this, a whole range of R&D work must be carried out, including a Phase I clinical trial.
In preparation for the prospective clinical trials, a comprehensive preclinical research program is to be conducted including further pharmacology, toxicology and ADME studies. The data collected during the preclinical studies will provide the basis for the design of clinical trial protocols, including the selection of the first dose, the design of the dose escalation regimen, as well as the selection of parameters to be monitored during clinical trials. The choice of doses and the dosing regimen should ensure that necessary exposure is achieved in humans, comparable to that at which a clear pharmacodynamic effect has been observed for in vivo models.
The demand for investigational substance increases as the project progresses. It is necessary to provide a required amount of the compound for toxicology studies, formulation development and manufacturing of the investigational medicinal product for clinical trials. In preparation for manufacturing the investigational substance and the investigational medicinal product in GMP standard for clinical trials, Pikralida’s specialists are pursuing advanced work on the development of a scalable process for the synthesis of clinical candidate PKL-021, and are soon to begin work on the development of formulations and manufacturing technology for the investigational medicinal product.
An important step of the project will involve the preparation of regulatory documentation and obtaining authorisations required by the pharmaceutical law for the prospective clinical trials to be launched. In order to obtain such an authorisation, first and foremost it must be demonstrated that the investigational medicinal product meets high quality standards, that its administration is justified by a medical need, and that the risk of administering the compound to humans is minimal. Pikralida estimates that a Proof-of-Concept Phase II clinical trial on a patient population will begin in 2024.
Drug repurposing or repositioning strategy consists in seeking new therapeutic indications for known medicinal products used in the clinical practice, as well as for drug candidates eliminated from clinical trials due to lack of therapeutic effect or unacceptable safety profile. The drug repurposing strategy is cost-effective, while projects based thereon carry lower risks compared to new drug development projects starting from scratch, i.e. the early drug discovery phase. Most importantly, the risk of project failure due to drug delivery safety issues is minimised, since the safety profile of the molecule had been characterised. Often, side effects that disqualify a drug from treating conditions that require long-term administration, such as diabetes, hypertension and cancer, may find use in treating disease entities that require short-term drug treatment. The biggest challenge of a successful drug repurposing strategy is to determine whether a particular molecule can be used in a new indication. Several methods have been developed to identify new therapeutic uses for known drugs and drug candidates. From the point of view of project launch, it is essential to verify scientific hypotheses, the potential of a given molecule as a drug for a new indication, by conducting biological experiments, such as in vivo models of a particular disease entity. The drug repurposing strategy is part of the European Commission’s Pharmaceutical Strategy for Europe.
The project carried out by the consortium of Pikralida sp. z o.o. and the Nencki Institute of Experimental Biology of the Polish Academy of Sciences, entitled “Use of matrix metalloproteinase inhibitor for the development of an innovative therapeutic method for preventing the development of post-injury and post-stroke epilepsy” is co-funded by the European Union under the Operational Programme Smart Growth 2014-2020. Project budget: PLN 21,564,812.50.

